|
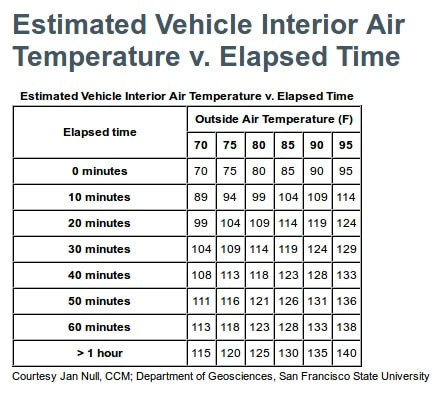
Brutus, Duke, Coco, Lola and Jake...sure, they're fairly common pet names, but they're also the names of just a few of the pets that died last year because they were left in cars on warm (and not necessarily hot) days while their owners were shopping, visiting friends or family, or running errands. What's so tragic is that these beloved pets were simply the victims of bad judgment. Want numbers? An independent study showed that the interior temperature of vehicles parked in outside temperatures ranging from 72 to 96° F rose steadily as time increased. And cracking the windows doesn't help. ...add to that the fact that most pets are not properly restrained while in the car, and you've got some dangerous situations – for people and pets alike. Unrestrained pets can be seriously or fatally injured, or could even hurt you, in a collision or sudden braking situation. In addition, they're a distraction for the driver, which increases the risk of driver errors. According to a 2010 American Automobile Association (AAA) survey, 2 out of 3 owners engage in distracting behaviors (playing with, feeding or petting their dog, or letting their dog sit in their lap) when pets are in the car...and according to the National Highway Traffic Safety Administration (NHTSA), approximately 20% of injury crashes involve distracted driving. Please don't become another statistic: only take your pets in the vehicle with you when you absolutely need to, and always properly restrain your pets while in the vehicle. How can you help prevent these injuries and deaths?
A Peaceful Farewell provides compassionate at home pet euthanasia to fellow pet owners in Chandler, Gilbert, Mesa, Tempe, Ahwatukee, Scottsdale, and most of the Greater Phoenix Metropolitan Area.
0 Comments
 Staph Infection in Dogs and Cats: Don’t Panic A staph infection in your dog or cat, thank goodness, is usually nothing to worry about — particularly if you get in to see your veterinarian as soon as you notice something is wrong. Bacteria of the genus Staphylococcus are what we call “ubiquitous.” In other words, staph is a very common bacteria that normally lives everywhere — in the environment, on the skin, and in the noses and mouths of our pets. High-risk Scenarios for Staphylococcal Infections in Pets Typically, a staph infection in your dog or cat is not troublesome. PHEW! That being said, staph infections are able to take advantage of certain situations and an infection can develop.This can make staphylococcus an “opportunistic pathogen.” It is most likely to take advantage of:
Signs and Symptoms of an Infection When staph causes an infection, we can see many different symptoms, which largely depends on which part of the body this opportunistic invader is invading. Symptoms can be classified into two main categories, namely “systemic” (affecting the whole body) or “specific.” Systemic signs of a staph infection can include:
These systemic symptoms are similar for nearly all infections. More specific symptoms of a staph infection might include:
In addition, approximately 8 to 10% of all urinary tract infections in pets are caused by “Staph.” Signs of a urinary tract infection include:
See Your Veterinarian! The most important thing to remember: if your pet is acting ill, see your veterinarian. As a responsible pet owner, it is wise to develop a relationship with a veterinarian you know and trust. That way, at the first sign of trouble you can get our pet treatment. Source: Trupanion.com / Denise Petryk, DVM A Peaceful Farewell provides compassionate at home pet euthanasia to fellow pet owners in Chandler, Gilbert, Mesa, Tempe, Ahwatukee, Scottsdale, and most of the Greater Phoenix Metropolitan Area.
 Humans with terminal cancers or with widespread metastases are offered treatment with the hope of an extended lifespan, despite a grim prognosis. People are routinely administered second, third, fourth, and beyond treatment plans when they fail to respond to the frontline therapies. This is done with little to no evidence-based information that would suggest such interventions will actually result in a positive outcome. The benefit of aggressive therapy in patients with terminal cancers is poorly described. The American Society of Clinical Oncology (ASCO) identified chemotherapy use among patients for whom there was no clinical value as “the most widespread, wasteful, and unnecessary practice in oncology.” When I read those words as a veterinary oncologist, I had only one thought. Ouch. The majority of patients I treat with cancer will ultimately succumb to their disease. Pets are typically diagnosed at an advanced stage of disease, and a cure is nearly impossible. We also accept much lower rates of toxicity with our chemotherapy protocols than our human counterparts; therefore, with good reason, we can’t treat animals’ cancers to the “fullest potential.” I would estimate that the premise of treatment for greater than 90% of cases I see is rooted in palliation (i.e., relief from pain) rather than a true belief of cure. Yet, veterinary oncology is fundamentally based on principles of human oncology. So if the data for human oncology tells us that the treatment of terminally ill cancer patients is not only poorly beneficial but also wasteful (in terms of not only finances but resources), how can I justify the recommendations I make each day? The answer is simple: Veterinary oncology is premised on the idea of treatment making our patients feel better, not worse. Rarely are animals diagnosed with cancer incidentally. Most show some sort of clinical signs prior to their diagnosis of cancer. Treatment, therefore, is aimed at relieving such signs and returning their quality of life to their baseline level. A study recently published in the Oncology edition of the Journal of the American Medical Association examined the evaluation of the use of chemotherapy and quality of life for people with end-stage cancer. Specifically, researchers were interested in knowing whether chemotherapy had a positive or detrimental effect during the last week of life for human patients with cancer, and if the effect was dependent on the patient’s overall health status prior to treatment. In people, performance status is used to evaluate a patient’s quality of life. There are several different scoring systems, with the Eastern Cooperative Oncology Group (ECOG) being widely accepted and outlined as follows: In the aforementioned study, a patient’s quality of life near death (QOD) was measured using a validated caregiver’s rating of their mental and physical distress during their final week of life. Results from the study raise several interesting points:
Despite the shared foundation of human and veterinary oncology, there is an enormous disparity between the end goals of each discipline. Human oncology is based on the concept of treating patients with the mantra of “life at all costs,” while veterinary oncology accepts our limitations, choosing to “maintain or improve quality of life” over cure. This is the message I attempt to relay during each new consultation I see. This is the information I am passionate about dispersing with my written and spoken dialogue each day. This is why I work so hard to help animals and their owners at every possible junction I am afforded. The battle to dispel the misconceptions about cancer care in animals is never-ending but worth enduring, knowing I can make a difference if even for just a few. Especially if the few are those who feel the “ouch” factor mentioned above just a bit deeper than all the others. Source: Pet MD / Dr. Joanne Intile A Peaceful Farewell provides compassionate at home pet euthanasia to fellow pet owners in Chandler, Gilbert, Mesa, Tempe, Ahwatukee, Scottsdale, and most of the Greater Phoenix Metropolitan Area.
We can’t live without water. But our waters can often be dangerous to us and our pets. A Florida television channel reported last week about the deaths of two men who had contracted a rare flesh destroying bacteria found in salt water. Six others were reported to have been stricken with the same bacteria. Whether the condition was contracted directly from the water, or from oysters or fish from those waters, is still not clear. There have been no reports of dogs being stricken by the same bacterial infection. The incident, however, got me to thinking about the many ways that water can harbor danger to our pets. This post will explore a few. Jellyfish Jellyfish washed onto the shore are a very common finding for beach combers and their beach combing dogs. The tentacles of these creatures have organs that release a stinging toxin whose potency varies with the different species of jelly fish. Even dried out tentacles in the sand or mixed in seaweed can still release the toxin. Dogs that come in contact with the tentacles or bite them can have a mild to serious local allergic reaction, or a more serious anaphylactic reaction resulting in shock. That is exactly what happened to 2-year-old pit bull named Diamond after she bit the tentacles of the most toxic of jellyfish, the Portuguese Man O’ War. After several days in intensive care, including transfusions, Diamond survived and is back to her old self. Many dogs are not that fortunate. If your dog has been stung by jellyfish tentacles, even one of the less toxic species, remove the tentacles without touching them directly with your bare hands and immediately seek veterinary care. Blue-Green Algae Warm weather can promote massive growth of blue-green algae in standing bodies of fresh or brackish (the slightly salty waters of lagoons, estuaries, and ponds near the ocean) waters. The musty or foul smell of the algae is often attractive to dogs. It can cause skin rashes for dogs swimming in the algae infested water. Dogs should be thoroughly washed as soon as possible. For dogs that drink algae contamintaed water, toxins in the algae can affect the kidneys, liver, intestines, and nervous system. Initial symptoms are vomiting, diarrhea, weakness, and difficulty walking. Immediate veterinary care is also advised in these cases. Parasites and Bacteria Standing areas of fresh water like small lakes, ponds, and even puddles can host various parasites and bacteria. Giardia and Cryptosporidium are the most common parasites. These parasites cause gastrointestinal distress resulting in vomiting and diarrhea. Most dogs recover quickly from the infection, but puppies and older dogs with compromised immune systems can be severely affected and need medications and diet modification in order to recover. Leptospirosis can also be found in small bodies of water that have been contaminated by rodents and other small animal that urinate in the water. Although not as common as water-borne parasites, the bacteria is much more dangerous to dogs that drink the contaminated water. Leptospirosis causes kidney damage that can lead to kidney and liver failure. Infected dogs may be lethargic and vomit. With early diagnosis and treatment, dogs do not suffer long-term kidney or liver problems. Vaccines are available to prevent the disease but they are somewhat controversial due to their tendency to cause allergic reactions and because of the vaccination frequency needed to effectively prevent the disease. Salt Water Poisoning Dogs love to frolic in the ocean, but salt water is toxic to humans and dogs if they drink too much. Ocean soaked tennis balls or other absorbent fetch toys contain enough salt to cause problems for the dogs that are fetching them. Mild ingestion of salt water can cause “beach diarrhea.” The excess salt (or hypernatremia) in the intestines draws water from the blood into the intestines, causing the diarrhea. The diarrhea can sometimes contain blood and mucous. If your dog drinks large amounts of salt water, hypernatremia can lead to vomiting, dehydration, incoordination, seizures, and require veterinary care. Avoid salt poisoning by taking a break every 15 minutes away from the water to offer fresh water to the dog. If your dog won’t drink willingly, use a bottle with a sports cap and squirt fresh water into the mouth. Water activity is great for dogs and the exercise far outweighs the risks, but it is important to be mindful of the risks in the water you dog so dearly loves. Source: Pet MD / Dr. Ken Tudor A Peaceful Farewell provides compassionate at home pet euthanasia to fellow pet owners in Chandler, Gilbert, Mesa, Tempe, Ahwatukee, Scottsdale, and most of the Greater Phoenix Metropolitan Area.
Though cat owners may want to depend on a cat to clean herself, there may be a time when you will want to give your cat a bath. The following tips will help you and your cat have a more pleasant experience. Prior to the bath, you will want to groom your cat. Use a grooming glove, fine-toothed comb, or soft brush for shorthaired breeds and a wide toothed comb and a soft slicker brush for longhaired breeds. Brush your cat thoroughly being especially gentle on the skin because it is thin and sensitive. Also, make sure to brush out any mats you may find - they are much harder to remove from wet hair. This is also a good time to check for sores, abscesses, lumps, and other skin problems. Clean your cat's ears and look for any excess wax or debris in the ears. You will also want to clip your cat's nails at this time. If your cat does not enjoy any of these procedures, wait until your cat has calmed down before starting the bath. Assemble all the materials you will need before you get the cat. Include a soft towel andshampoos and conditioners formulated especially for cats. If the shampoo is very thick, it is sometimes helpful to dilute it with some water before applying it to the cat. Just prior to the bath, place cotton balls in the ears and apply ophthalmic ointment to protect the eyes. Place a towel in the bottom of the sink or tub you are going to use to prevent slipping. Be sure the area where you give the bath is warm, and your cat will have a warm place to dry off. Remember that cats do not like to be restrained, so the less she feels like you are controlling her, the better. Speak in soft tones and try to appear calm, since your cat will become more nervous if she senses you are apprehensive. Signs that your cat is anxious include flattening of the ears or whiskers, tail thumping, loud vocalizations, and open mouth panting. Use lukewarm water. Cats generally dislike sprays, so it is often better to pour water over the cat rather than spraying. If you must spray, avoid hard sprays and spraying near your cat's face. You may want to wrap your cat in a thin towel and wet the coat through the towel, remove the towel, and then apply the shampoo. After shampooing, rinse your cat thoroughly. Rinsing is the most important step. The old adage is: 'Once you think you've rinsed your cat thoroughly, rinse her again.' Dry your cat gently with a towel. 'Blotting' is better than rubbing, especially in longhaired breeds. Longhaired breeds will also benefit from an additional brush out and a blow dryer on no-heat setting (if your cat will tolerate the noise). If your cat absolutely cannot tolerate being wet, try using a waterless or powder shampoo, pre-moistened bath towelettes for pets, or give your cat a 'sponge bath' with a damp towel. Remember, the younger a cat is when you begin to bathe her, the more likely it will be that she will come to enjoy an occasional bath. Source: peteducation.com A Peaceful Farewell provides compassionate at home pet euthanasia to fellow pet owners in Chandler, Gilbert, Mesa, Tempe, Ahwatukee, Scottsdale, and most of the Greater Phoenix Metropolitan Area.
 What’s Causing the Dog Hair Loss? Seeing a dog lose his or her hair can be disconcerting to witness. However, what’s most important when dealing with alopecia, as it is referred to medically, is identifying the underlying cause of the hair loss in order to devise an appropriate treatment plan. Here are five common culprits of hair loss in dogs that should be discussed with your veterinarian. 1. Allergies Allergies are a frequent cause of hair loss in dogs. This may due to environmental triggers such as pollen, molds and dust mites, or due to parasitic triggers like fleas or mites. Food allergies are another possible cause of hair loss. Typical symptoms of an adverse allergic reaction include itchiness resulting in excess scratching, biting, and, of course, hair loss. In the case of flea allergies, it is recommended that dogs take flea preventatives as a way to minimize threats of a full-blown flea infestation. 2. Infection or Infestation An infestation with parasites such as fleas, ticks, and mites (scabies, mange) is another source canine alopecia. Along with hair loss around the ears, eyes, abdomen, and chest, signs your dog may have mites or fleas/ticks include inflammation, itching and redness. Bacterial or fungal infections, such as in the case of ringworm (which is actually a fungus), can also be attributed to hair loss in dogs. Symptoms of ringworm include circular or irregular hair loss, inflammation, and infected crusts. 3. Cushing's Disease Hyperadrenocorticism, also known as Cushing's disease, is a condition caused by the prolonged exposure of the body’s tissue to excessive levels of the hormone cortisol. Symptoms of Cushing’s disease include hair loss, darkening of the skin, and the development of a pot-bellied abdomen. Cushing’s disease commonly occurs in middle-aged to senior dogs, though it can also affect dogs that overuse corticosteroid drugs. 4. Genetics There are some breeds of dog that are more genetically prone to baldness than others. First there are the hairless dogs that have been bred for the attribute such as the Chinese Crested, Mexican Hairless (Xolo), and American Hairless Terrier. Other dog breeds, such as the Doberman Pinscher, Dachshund, Chihuahua, Italian Greyhound and Whippet, sometimes suffer from patchy or pattern baldness on the outer ear, chest, back, thigh, or lower neck. 5. Pressure Sores Pressure sores, also called bedsores or decubital ulcers, are localized injuries where the dog’s elbows or other bony pressure points (hips, hocks, etc.) come into contact with hard surfaces regularly. This constant pressure and friction causes the skin to callus, lose hair and sometimes crack and bleed. Pressure sores are more common older dogs, especially large or heavy breeds. A Peaceful Farewell provides compassionate at home pet euthanasia to fellow pet owners in Chandler, Gilbert, Mesa, Tempe, Ahwatukee, Scottsdale, and most of the Greater Phoenix Metropolitan Area.
 Hyperthyroidism is the most common hormonal abnormality in cats, causing the thyroid gland to become overactive and produce excess amounts of thyroid hormone. Fortunately, a more recent discovery has made the way to treat the disease easier for veterinarians, while also making the costs of treatment less expensive on the cat owner. Traditional treatments included radioactive iodine treatment to inactivate the tumor cells that cause excess secretion of thyroid hormone, or medication to suppress hormone secretion. Several years ago, it was found that a limited iodine diet was just as effective as the traditional methods of treating hyperthyroidism in cats. The solution was revolutionary and substantially reduced the costs of treating this condition. Hyperthyroidism and Limited Iodine Diets for Cats The thyroid hormone regulates body metabolism. Older cats with microscopic tumors of the thyroid gland secrete excess thyroid hormone, which increases metabolism. This excess secretion results in an increased appetite with weight loss. Affected cats often beg for more food and arouse owners late at night with howls of hunger. These cats also drink lots of water and have increased urination. The increased metabolic rate also causes an increased heart rate and an eventual heart murmur due to heart malfunction. The increased metabolic rate also affects kidney function and these cats are often in secondary kidney failure when the condition is diagnosed. Recent research found that limiting iodine in the diet of hyperthyroid cats decreased thyroid hormone production and the resulting harmful side effects. This treatment approach was more affordable and as reliable as the traditional treatment methods. The proof is in the research. Research Findings on Limited Iodine Diets for Cats A study published in the International Journal of Applied Research last year (A Restricted Iodine Food Reduces Circulating Thyroxine Concentrations in Cats with Hyperthyroidism) found that after being fed a limited iodine diet over a 12-week period, half of the cats with hyperthyroidism at the beginning of the study were euthyroid, or had normal thyroid gland function. The randomized and blinded study enrolled 33 cats – 18 on the restricted iodine diet and 15 in the control group. These results show that over 12 weeks, feeding a limited iodine food reduces serum thyroid hormone concentrations in hyperthyroid cats without negatively affecting other measures of health. Feeding a limited iodine food warrants further study as a treatment option for feline hyperthyroidism. Will Limited Iodine Diets Harm My Other Cat(s)? At the Academy of Veterinary Internal Medicine Symposium last year, I had an opportunity to meet with scientists who had developed the limited iodine diet and had done research into the effects of this diet on normal cats. Their findings were extremely encouraging. Admittedly, their research population was limited, with 15 cats receiving a diet with adequate iodine and 15 receiving limited amounts of iodine. But they did extend the research period to 18 months. This is far longer than most nutritional studies. Their findings concluded that no health problems were noted for healthy cats on a limited iodine food. The researchers admit that longer studies are necessary to conclusively prove that iodine-deficient diets are safe for normal cats. However, this research suggests that owners of a hyperthyroid cat in a multi-cat household do not have to make Herculean efforts to ensure dietary segregation and can even feed the same food for all members of the household. Of course, caution should be taken for kittens exposed to limited iodine diets. Their sensitivity could certainly result in problems and access to limited iodine foods should be restricted until research in this group has been conducted. Source: PetMD / Dr. Tudor A Peaceful Farewell provides compassionate at home pet euthanasia to fellow pet owners in Chandler, Gilbert, Mesa, Tempe, Ahwatukee, Scottsdale, and most of the Greater Phoenix Metropolitan Area.
Buying Flea and Tick Medicine for a Dog? Read This First!With so many brands and types of flea and tick medications being sold today, it can be rather overwhelming choosing what's best for your dog. Here are a few important things to consider before grabbing the first flea and tick control product you see. 1. Usage Flea and tick control products come in a variety of forms, including foggers, wipes, dips, shampoos, spot-ons, collars and oral medication. Some products repel fleas and ticks; some attack the immature forms of the bugs so that they never have a chance to develop and reproduce; and others kill the adult fleas and ticks. There are even some products that do all three. Read the label carefully to select the best product for your situation, and consult your veterinarian if you have any questions. 2. Flea/Tick Species Effectiveness It may be a bit overwhelming to think about, but there are hundreds upon hundreds of flea and tick species worldwide! The dog flea, black-legged tick (pictured above), American dog tick and brown dog tick, just to name a few. Discuss with your veterinarian what type of fleas and ticks are found in your area and confirm that the flea and tick medicine you're considering is effective against those species. Look for medications labeled "broad spectrum," which are effective against several species in one easy-to-use form. 3. You and Your Dog's Preferences Another important consideration is you and your pet's preferences and lifestyle. Perhaps your dog isn't very fond of having spot-on flea and tick preventives and won't stay still during application. Try a flea and tick collar. What if you have a busy lifestyle and want something that is both effective for long periods and that isn't visible on your pet? Check out oral flea and tick preventives (i.e., pills or tablets), as some are effective for up to 12 weeks. There isn't necessarily a right or wrong choice when it comes to choosing flea and tick medication. Just choose what is best for your situation. 4. Intended for Dogs or Cats? There are times when dogs and cats can take the same medication, under a vet's supervision, to resolve an issue. This is definitely not one of them. Not only are some flea and tick medications specifically formulated to be effective for dogs (or vice versa); there are certain ingredients that can actually be harmful, even deadly, to cats. "Cats should never be given products designed for use on dogs," says Dr. Jennifer Kvamme, DVM, "nor should you use your cat products on your dog." Always read flea and tick control products labels carefully and only use as directed. If you have any doubts, ask your veterinarian. A Peaceful Farewell provides compassionate at home pet euthanasia to fellow pet owners in Chandler, Gilbert, Mesa, Tempe, Ahwatukee, Scottsdale, and most of the Greater Phoenix Metropolitan Area.
 With Easter coming up here is a quick reminder that Easter Lily is poisonous to cats. Poisonous to: Cats Level of toxicity: Generally moderate to severe Common signs to watch for:
There are benign and dangerous lilies out there, and it’s important to know the difference. Benign lilies include the Peace, Peruvian, and Calla lilies; these contain insoluble oxalate crystals that cause minor signs such as tissue irritation to the mouth, tongue, pharynx, and esophagus. Clinical signs of drooling, pawing at the mouth, foaming, and vomiting may be transiently seen. The more dangerous, potentially fatal lilies are true lilies of the Lilium or Hemerocallis species. Examples of some of these dangerous lilies include the tiger, day, Asiatic hybrid, Easter, Japanese Show, rubrum, stargazer, red, Western, and wood lilies – all of which are highly toxic to cats! Even small ingestions (such as 2-3 petals or leaves) – even the pollen or water from the vase – can result in severe, acute kidney failure. Other types of dangerous lilies include lily of the valley. This type does not cause kidney failure, but can cause life-threatening heart arrhythmias and death when ingested by dogs or cats. If your cat is seen consuming any part of a lily, bring your cat (and the plant) immediately to a veterinarian for medical care. The sooner you bring in your cat, the better and more efficiently the lily poisoning can be treated. Decontamination (like inducing vomiting and giving binders like activated charcoal) are imperative in the early toxic stage, while aggressive intravenous fluid therapy, kidney function monitoring tests, and supportive care can greatly improve the prognosis. Intravenous fluids must be started within an 18 hour window for the best outcome. Poison type: Plants Scientific name: Lilium longiflorum Alternate names: Lilies, Easter lily, tiger lily, rubrum lily, red lily, wood lily, Western lily, stargazer lily, daylily, Japanese show lily, Asiatic lily, Asiatic hydrid lily, peace lily, calla lily, lily of the valley, Lilium longiflorum, Lilium tigrinum, Lilium speciosum, Lilium auratum, Lilium lancifolimu, Lilium umbellantum, Hemerocallis Source: http://www.petpoisonhelpline.com/ A Peaceful Farewell provides compassionate at home pet euthanasia to fellow pet owners in Chandler, Gilbert, Mesa, Tempe, Ahwatukee, Scottsdale, and most of the Greater Phoenix Metropolitan Area.
by Dr. Joanne Intile, DVM Many owners administer herbal supplements to their pets with cancer with the hope that these alternative therapies will afford their pet a therapeutic edge in fighting the disease. The amount of information suggesting the beneficial effects of various herbs, anti-oxidants, “immune boosting treatments,” and dietary supplements is astounding. The appeal of using a substance that is “natural” and “non-toxic” to disease is inarguably real. What most owners fail to recognize is that herbal medications are not subject to the same regulations by the Food and Drug Administration (FDA) that prescription drugs are. Owners are also unaware that carefully worded claims to efficacy are not backed up by scientific research in the vast majority of cases, despite the plethora of supportive material listed on product inserts or on websites. Legally, herbal supplements are considered “foods” and not “drugs.” Therefore, the FDA has minimal regulatory role over their production and advertising. The FDA acts to ensure that there are no overtly misleading claims made by the manufacturer, and also mandates that it is illegal for a product sold as a dietary supplement to be promoted on its label, or in any of its labeling material, as a “treatment, prevention, or cure for a specific disease or condition.” Dietary supplements do not need approval from the FDA before they are marketed. Except in the case of a new dietary ingredient, where pre-market review for safety data and other information is required by law, a firm does not have to provide the FDA with the evidence it relies on to substantiate safety or effectiveness before or after it markets its products. A recent investigation was conducted by the New York State Attorney General’s office examining the integrity of various herbal supplements via DNA analysis of their ingredients. Results astonishingly showed that 4 out of 5 herbal products were found to contain none of the herbs listed on the ingredient label. From the press release from the New York State Attorney General’s office: Overall, just 21% of the test results from store brand herbal supplements verified DNA from the plants listed on the products’ labels — with 79% coming up empty for DNA related to the labeled content or verifying contamination with other plant material. … 35% of the product tests identified DNA barcodes from plant species not listed on the labels, representing contaminants and fillers. A large number of the tests did not reveal any DNA from a botanical substance of any kind. Some of the contaminants identified include rice, beans, pine, citrus, asparagus, primrose, wheat, houseplant, wild carrot, and others. In many cases, unlisted contaminants were the only plant material found in the product samples. Though the results of the investigation are concerning, one could argue a lack of accuracy in product integrity would do little harm other than waste the buyer’s money. As a veterinarian, what I worry about is whether what’s actually present in the supplement could be detrimental to my patient’s health. Could these non-listed ingredients cause a severe allergic reaction in an animal? Could these additional ingredients interact negatively with a previously prescribed conventional treatment? Are they really safe? I’m not arguing against using natural substances to treat disease. In fact, one of the most common chemotherapy drugs I prescribe is vincristine, a drug derived from the periwinkle plant. Aspirin was originally produced from salicylate containing plants such as the willow tree. And on a personal account, ginger is a definite anti-nausea remedy for my own occasionally sour stomach. But I also know that many natural substances can be extremely toxic for pets. There are many species of poisonous wild mushrooms; botulin toxin (aka “Botox”) is natural, but can be deadly for animals; and yes, even the vincristine I prescribe routinely to my patients can be deadly if proper dosing is not maintained. I’m concerned that owners are wasting their money on supplements touted as cure-alls for their pets. I worry that these substances could actually be causing harm to my patients because of unknown ingredients that interact negatively with prescribed medications or with that animal’s particular physiological constitution. And I have concerns that the average consumer isn’t aware of the lack of regulation of these substances, which is the impetus for writing this article. Be sure to speak directly with your veterinarian in reference to your questions about supplements and their potential role in your pet’s healthcare. And be sure to let your pet’s doctor know about any supplements, vitamins, and other over the counter remedies you may be administering to your pet. An open dialogue is essential for making the best decisions about your furry companion’s well being. To learn more, visit the American Cancer Society’s information page on supplements: Dietary Supplements: What is Safe? Source: PetMD A Peaceful Farewell provides compassionate at home pet euthanasia to fellow pet owners in Chandler, Gilbert, Mesa, Tempe, Ahwatukee, Scottsdale, and most of the Greater Phoenix Metropolitan Area.
|
The PAW Blog...
For the LOVE of Pets The goal of this blog is to help educate pet owners by sharing pet health facts and pet news articles...and ... sometimes put a smile on your face with a cute or funny pet story! Categories
All
Archives
July 2024
Search for any topic...
|



 RSS Feed
RSS Feed